A Runner's Guide to ITBS
by Ann Schofield, P.T., MCSPIliotibial band syndrome (ITBS) is the most common cause of pain on the outside of the knee in runners, with an incidence as high as 12% of all running-related overuse injuries. Although it is not difficult to diagnose, it can be a challenge to treat, especially in higher mileage runners who place enormous loads on their bodies. This article has been written to help the runner diagnose, understand and begin to treat IT band friction syndrome.
WHAT IS THE ILIOTIBIAL BAND?
The IT band is not a muscle. It is a thick band of tissue called fascia that starts on the outside of the hip, passes down the outside of the thigh and inserts into the side of the patella (knee cap) and the tibia, (shin bone).
Fascia is a sheath-like tissue that surrounds muscles. The ITB has the tensile strength of soft steel, which explains why it is so difficult to mobilize.
As well as arising from the iliac crest, (hip bone) the ITB attaches into the gluteal muscles at the back and tensor facia lata muscle at the front. (See Figure 1)
When these muscles contract, they increase tension on the band. Often, one muscle dominates the movement pattern causing an imbalance to occur, which may lead to injury.
WHAT ARE THE SYMPTOMS OF ITBS?
- Pain from the ITB is easily recognized as a sharp or burning pain on the outside of the knee when running. Typically, an athlete is unable to “run through” ITB pain.
- Early on, symptoms will subside shortly after the run is over, but will return with the next run, usually after a reproducible amount of time.
- Later, if there has been no positive intervention, the pain may come on sooner and persist with walking or going up and down stairs.
- Tenderness may be felt on the outside of the knee when pressure is applied, especially when the knee is slightly bent.
- There is not usually any swelling associated with this problem, but the band itself may be thickened.
WHY DOES IT HURT?
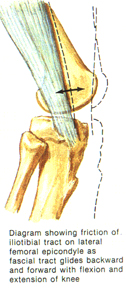
As the knee bends, tension acting on the band, causes it to be pulled backwards over the lateral femoral epicondyle, (a bony prominence of the thigh bone on the outside of the knee). When the knee straightens, tension on the band pulls it forward again. A thin bursa, or fluid filled sac, separates the ITB from the femoral epicondyle, to decrease friction between these structures. Repetitive bending and straightening of the knee can cause inflammation of the bursa and the band itself, or irritation of the bone due to recurrent rubbing or impingement. (See Figure 2)
WHAT CAUSES ITBS?
A number of etiologic factors have been related to ITBS in runners, but it is important to understand the cause is probably multifactorial. Weekly mileage will interact with a combination of biomechanical issues, training strategies, as well as variables imposed by an individual’s specific muscle imbalances; once critical threshold is met, tissue breakdown will occur. It is not necessary to sustain a specific traumatic injury to the knee for the ITB to become a problem.
COMMON STRESSORS WHICH MAY IMPACT THE DEVELOPMENT OF ITBS
INTRINSIC FACTORS
- Tightness in the iliotibial band.
- Myofascial restrictions in the hip and thigh musculature, which will increase tension on the band.
- Weakness in hip abductors, (common in distance runners).
- Weakness or poor control of knee muscles, especially the quads.
- Dominance of anterior hip muscles, (TFL) over posterior hip muscles, (glutes).
- Excessively flat feet or high arches.
- Bow legs or knock-knees.
- Leg length inequality.
- Limited ankle range of motion.
EXTRINSIC FACTORS
- Training errors e.g. Excessive mileage, sudden increase in mileage, sudden increase in intensity of training, too much hill work, running on crowned roads
- Over striding
- Worn out running shoes
- Failing to warm up or cool down properly
All of the extrinsic and most of the intrinsic contributors can be addressed to minimize stress on the ITB and reduce the risk of injury.
CHECKLIST FOR THE PREVENTION OF ITBS
- Change running shoes every 300 to 500 miles, or every 3 to 4 months, when they have lost approximately 40 to 60 percent of their shock absorbing abilities. High mileage runners should have two pairs of shoes to alternate between, to allow 24 hours for the shock absorbing material to return to its optimal form. Do not underestimate the importance of good shoes in the prevention of many types of injuries. It’s worth the cost in the long run.
- Always slowly increase running mileage and if adding hills, do so gradually. Downhill running especially increases friction on the ITB as well as fatiguing the quadriceps, which are the main stabilizers of the knee. If too tired they will not be able to control the knee position and this may lead to unwanted stress and injury.
- Avoid training on uneven surfaces, as the down leg may be predisposed to ITBS.
- Always keep the knees warm. ITB seems to react adversely to cold, so cover up your knees when running outdoors if it’s below 60 degrees.
- After a run, cool down and stretch; ice if necessary.
TREATMENT AND REHABILITATION
Rehabilitation is aimed at reducing inflammation, restoring flexibility of the ITB and improving overall control, muscle imbalance and alignment of the lower extremity and foot.
ACUTE PHASE
- Activity modification is essential to reduce friction to the band. Try cross training into other aerobic activities that don’t cause pain during or after activity. Pool running may work despite the fact the band is still moving over the epicondyle because it is non-weight bearing. This will take tension off the band. Swimming with a pool buoy between the legs will reduce any mechanical irritation completely and may be best for the first few days.
- The elliptical machine and cycling may be attempted, as the biomechanics are different from running even though the knee is bending and straightening, but if pain does occur discontinue.
- Everyone is different, depending on the level and exact mode of inflammation, tolerance to cross training will vary. In this author’s opinion, if it doesn’t hurt before or after activity, then it should be OK to continue. Sometimes “a change is as good as a rest.”
- Ice! Ice! Ice! Ice applied locally for 10 minutes at a time should be carried out at least 4 times a day. Ice will help to reduce inflammation and will continue to be beneficial throughout the course of treatment.
- Oral nonsteroidal anti-inflammatory medications, such as Motrin may help reduce pain and inflammation. Generic brands of Ibuprofen are exactly the same and therefore equally as effective as the more expensive name brand “Motrin”, so save your money and buy in bulk.
- Sleep with a pillow between the knees to decrease tension on the ITB.
SUB ACUTE PHASE
- Soft tissue treatments, such as massage and release of myofascial restrictions can be started once the acute phase has subsided. This may be performed by a physical therapist or massage therapist.
- An effective way to address tight areas and trigger points independently, is to purchase a foam bolster and to apply direct pressure to problem areas by rolling back and forth, emphasizing those tight painful spots. This will help release the tight tissue, and will decrease tension on the band; consequently a significant part of the pain pattern will be reduced. (See Figure 3)
- Stretching exercises are usually necessary to lengthen the ITB, which is found to be contracted in most individuals with this problem. However, the ITB is a difficult structure to stretch effectively for the following reasons:
- The ITB does not have stretch receptors, in other words, it is not ‘stretch sensitive’, and therefore it is difficult for the athlete to know if the stretch is effective while it is being performed. The sensation of stretch may be coming from neighboring tissues and is misleading.
- Most of the “old school” ITB stretches documented and passed down from athlete to athlete are inadequate. They fail to stretch the band along its entire length. Because the ITB passes over more than one joint, it is very difficult to lengthen without compensations.


ILIOTIBIAL BAND STRETCH
- Sit on the edge of a table or firm bed.
- Roll back pulling the unaffected leg to the chest to flatten out the low back.
- Lower the affected leg to the table and bend the knee to 90 degrees.
- Now, without allowing the lower leg to rotate or twist, move the thigh across the midline. As you do this, do not let the thigh rise up from the table, it needs to stay down to stretch the ITB over the hip joint. Hold for 20 to 30 seconds, repeat 3 to 5 times. (See Figure 4)
The sensation of stretch may vary from one individual to another due to the absence of stretch receptors in the band. Some will feel a pull on the inside of the kneecap, which will go away once the stretch is over.
Ideally the band is warmed prior to stretching. This can be done with heating pads or a warm shower. Alternatively stretching can be carried out after a work out.
STRENGTH & STABILITY PHASE
An athlete is most likely to be successful returning from injury if specific weakness or muscle imbalances have been addressed. As the ITB arises from muscles in the hip, the relative control and stability these muscles offer will directly affect the more “passive” IT band. Runners with ITB problems have weaker hip muscles than those without this particular problem. It has been well documented recently that core strength and stability can help reduce injury and improve efficiency and performance. The following are three exercises that will improve control of the pelvis, hip and knees:
1. BRIDGING WITH SINGLE LEG RAISE
This exercise is great for improving a runner’s pelvic stability and hip control. It strengthens the gluts, obliques and thigh muscles while teaching them to work together efficiently for a strong core.
- Lie on back with hands resting on hipbones.
- Lift pelvis and shift weight slowly onto one foot.
- Extend the other leg, but do not allow the pelvis on this side to drop, your hands should remain level.
- Hold for 10 seconds, lower the pelvis back down and repeat on the other side. (See Figure 5)
- Repeat with other leg.
- Work up to 10 repetitions on each leg.
- Remember that quality of movement is important, so stop sooner if you’re unable to be stable.


2. CLAM SHELL
This exercise improves the control and function of the gluteus medius, a muscle found to be weak in distance runners with ITBS. By working it in this way, the balance between the anterior and posterior hip muscles will be restored. It is not OK to substitute this exercise for the multi hip machine at the gym!
- Lie on side with hips at 45 degrees and knees at 90 degrees.
- Keep heels together and lift upper knee by turning out at the hip. (See Figure 6)
- It is essential to keep the pelvis perpendicular to the bed rather than rolling backwards. Hold for 10 seconds; work up to 10 repetitions.
- Repeat other side.
3. STEP DOWNS
This exercise will improve knee control and strengthen the quads for downhill running and softer more economical running.
- Choose a stable step 2” to 6” in height.
- Step down from the step slowly. (See Figure 7)
- Your knee should follow the toes and should not knock in towards the other knee.
- Use a mirror to check that the pelvis stays level, it may help to place hands on hipbones to monitor this. Work up to 3 sets of 10.
If this exercise is too easy, then you’re not performing it slowly enough. With all three exercises, compare left and right sides. Are there asymmetries? Is one side harder to do properly than the other? Stay focused and concentrate on form.

RETURN TO RUNNING PHASE
Returning to running will vary from one individual to another, depending on the severity of the problem and the pre injury condition of the runner.
- Most importantly, remember that returning to running after injury is an art. The tissues need to be coaxed back to health. They need enough stimulus to adapt positively to the demands of running, but if loaded too much, will continue to negatively react by breaking down further, thus increasing the time of recovery.
- Running can be attempted when there is no pain with walking and generally the level of inflammation seems to be down (i.e. less discomfort when exercises are performed).
- Start with easy sprints on level ground, as studies show that running at a faster pace is less likely to aggravate the ITB than slow paced running. Recover between intervals by walking rather than jogging.
- Run every other day for the first week, then gradually increase distance and frequency as tolerated. Vary the speed of these runs to avoid placing too much stress on one primary area of inflammation. Cross training will help maintain aerobic capacity on the off days and allow the ITB to settle between runs.
- Do not add intensity or hill workouts until you have been symptom free for 3 to 6 weeks and have re established an adequate base.
- Initially it may be better to choose softer surfaces to run on for extra cushioning; training on firmer surfaces may follow as symptoms tolerate.
CORTIOSTEROID INJECTION
Cortisone injection is an option for those not responding to therapy, or athletes needing immediate relief to meet race obligations.
SURGICAL MANAGEMENT
Surgery is only rarely required for treatment of Iliotibial band friction syndrome. It is usually only necessary for those athletes unwilling to modify their activity level, or professionals unable to afford time off from training. It involves excision of a small portion of the band over the femoral epicondyle.
PEP TALK
It will help to consider those first early runs as “therapy” for the injured limb, rather than training for improved performance. To be limited to a five minute run is frustrating and may seem like a waste of time unless you keep in mind the real purpose of the run.
When returning from any injury, go out with a positive attitude and keep the specific goal for that particular run in mind. You’re out there for rehabilitation, not a personal best. This run has its place just like any other run in your program. Understand the necessity for gradual return and set yourself up for success.
It’s tempting to run for longer than planned, especially if you feel good, but you can do that the next time out. Respect the limitations your injury has placed upon you and you’ll recover faster. We often have to learn the hard way; instead try learning the smart way.
A full lower extremity examination is ideal to fully implement an effective program, specifically for an individual’s needs. To optimize your alignment, muscle balance and stability with movement, call or email for an appointment:
DYNAMIC CONTROL PHYSICAL THERAPY
Ann Schofield, RPT
Email FYSIO@COMCAST.NET
Phone (970) 226-5840
Cell (970) 581-0467
REFERENCES
- Comerford M, Dynamic control and muscle balance of the lower quadrant. Kinetic control movement dysfunction course, 2001
- Ekman EF, Pope T, Martin DF, et al: Magnetic Resonance Imaging of iliotibial band syndrome. American Journal of Sports Medicine 1994 851-854
- Fredericson M, Cookingham, CL, Sahrmann SA, et al: Hip abductor weakness in distance Runners with iliotibial band syndrome. Clinical Journal of Sports Med 2000: 169-175
- Fredericson M, Guillet M, DeBenedictis L: Quick solutions for iliotibial band syndrome. Physician & Sportsmedicine 2000 Volume 28
- Messier SP, Edwards DG, Martin DF, et al: Etiology of iliotibial band friction syndrome in distance runners. Med Sci Exer 1995: 951-960
- Kendall FP, McGreary EK, Provance PG. Muscles: Testing and Function, 4th ed. Baltimore: Williams & Wilkins, 1993
- Noble CA, The treatment of iliotibial band friction syndrome, British Journal of Sports Medicine 1979 51-54
- Orchard JW, Fricker PA, Abud AT, Mason BR: Biomechanics of iliotibial band friction syndrome in runners. American Journal Sports Medicine 1996: 375-379
- Sutker AN, Barber FA, Douglas W, et al: Iliotibial band syndrome in distance runners. Sports Medicine 1985 447-451
- Terry GC, Hughston JC, Norwood LA, The anatomy of the iliopatella band iliotibial tract. American Journal of Sports Medicine 1986 39-45